Misdiagnosis rates in adolescent mental health are a growing concern due to diverse symptom presentations across age groups and cultures. Cognitive Behavioral Therapy (CBT) is a popular but not universal solution, highlighting the importance of emotional intelligence and cultural sensitivity in mental healthcare. Burnout prevention among healthcare providers is crucial as fatigue or inexperience can hinder accurate diagnoses. Early intervention through CBT-based therapy programs empowers teens with emotional regulation skills, improving diagnostic accuracy and patient outcomes, especially when combined with continuous training for mental health professionals.
Mental illness diagnosis accuracy is a critical aspect of effective treatment, yet challenges like high misdiagnosis rates persist. This article delves into strategies aimed at enhancing diagnosis precision, focusing on innovative techniques such as Cognitive Behavioral Therapy (CBT) tailored for adolescent teens. We explore how CBT, combined with early intervention and continuous training, can significantly improve mental health diagnosis accuracy. Understanding the current landscape involves examining factors affecting diagnostic accuracy, paving the way for more effective support systems.
- Understanding the Challenges: Misdiagnosis Rates and Factors Affecting Accuracy
- Innovative Approaches: Enhancing Diagnosis Techniques with Cognitive Behavioral Therapy for Adolescent Teens
- The Impact of Early Intervention and Continuous Training on Improving Mental Health Diagnosis Accuracy
Understanding the Challenges: Misdiagnosis Rates and Factors Affecting Accuracy

Misdiagnosis rates in mental health are a significant concern, with studies showing that many individuals, especially adolescents and teens, receive incorrect or delayed diagnoses. This is a complex issue, influenced by various factors. One key challenge lies in the diverse presentation of symptoms across different age groups and cultural backgrounds. What may be indicative of one disorder in a young adult could be interpreted differently in a teen, leading to missteps in diagnosis.
Cognitive Behavioral Therapy (CBT), while effective for many, might not be suitable for all, and its application should consider emotional intelligence and cultural sensitivity in mental healthcare practice. Burnout prevention among healthcare providers is another critical aspect; fatigued or inexperienced professionals may fail to recognize subtle cues or attribute symptoms to underlying conditions, further complicating accurate diagnosis.
Innovative Approaches: Enhancing Diagnosis Techniques with Cognitive Behavioral Therapy for Adolescent Teens

Mental health professionals are continually seeking innovative approaches to improve diagnosis accuracy for adolescent teens, a demographic where mental illness often presents uniquely. Cognitive Behavioral Therapy (CBT) has emerged as a powerful tool in this regard, offering not just a structured framework for identifying symptoms but also a holistic understanding of their underlying causes. CBT focuses on the relationship between thoughts, feelings, and behaviors, empowering teens to challenge negative thought patterns and adopt healthier coping mechanisms.
Integrating compassion cultivation practices within CBT sessions further enhances the therapeutic experience. By fostering emotional healing processes, healthcare provider cultural competency training becomes invaluable. This training equips professionals with the skills to recognize and navigate cultural nuances, ensuring that every teen receives a diagnosis based on their individual experiences and backgrounds. Such personalized approaches not only improve diagnostic accuracy but also build trust between teens and their mental health caregivers.
The Impact of Early Intervention and Continuous Training on Improving Mental Health Diagnosis Accuracy

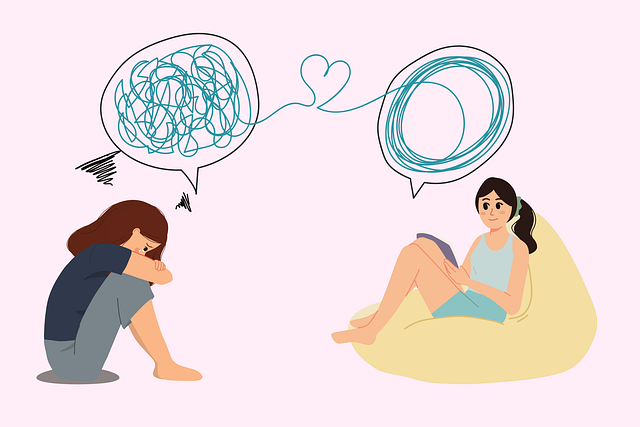
Early intervention plays a pivotal role in enhancing the accuracy of mental health diagnoses, especially for adolescents and teens. By implementing therapy programs like Cognitive Behavioral Therapy (CBT), healthcare providers can effectively support young individuals struggling with emerging mental health issues. CBT is known to empower patients with emotional regulation skills, enabling them to manage their symptoms and improve overall well-being. This proactive approach not only ensures timely intervention but also fosters better diagnostic accuracy by addressing the root causes of distress.
Continuous training programs designed for healthcare providers are another crucial component in this process. These programs focus on updating clinical knowledge, refining assessment techniques, and promoting burnout prevention strategies. By regularly educating professionals about the latest research, treatment modalities, and potential challenges in mental health diagnosis, we can ensure they remain adept at recognizing and accurately diagnosing various conditions. Such efforts contribute to a robust Mental Health Policy Analysis and Advocacy, ultimately leading to better-equipped healthcare systems and improved patient outcomes.
Mental illness diagnosis accuracy is a multifaceted challenge, with misdiagnosis rates highlighting the need for improvement. By understanding the factors affecting accuracy, such as comorbidity and individual presentation, we can implement innovative approaches like incorporating Cognitive Behavioral Therapy (CBT) tailored for adolescent teens. Early intervention and continuous training are game-changers in enhancing diagnosis techniques, ensuring more effective treatment plans. These efforts collectively contribute to improving mental health diagnosis accuracy, ultimately fostering better outcomes for individuals navigating their mental health journeys.